Quick Overview
-
Synthetic estrogens are found in hormonal contraceptives and menopause therapies.
-
In birth control, estrogen's main role is to regulate and predict bleeding.
-
Synthetic estrogens can cause both beneficial and adverse side effects.
What Is Estrogen?
Estrogen is one of the body’s most essential hormones. It plays a critical role in reproductive health, regulating the menstrual cycle, puberty, pregnancy, and more.
Hormones act as the body’s chemical messengers. Estrogen binds to specialised receptors in various tissues to activate specific physiological processes. Think of it as a key fitting into a lock: once it connects, the door to important body functions opens.
Natural vs. Synthetic Estrogen
Your body naturally produces endogenous estrogens, primarily estradiol — the most biologically active form. In contrast, synthetic (exogenous) estrogens are lab-made compounds used in medications to mimic the effects of natural estrogen.
These synthetic forms differ slightly in structure, influencing how they are absorbed, metabolised, and excreted. They may also activate estrogen receptors differently, leading to varied effects across individuals.
Natural support alongside HRT
While hormone replacement therapy can relieve menopause symptoms, many individuals seek complementary support to balance hormones, support mood, and protect bone and cardiovascular health. MENO Blend is crafted specifically for postmenopausal needs—containing phytoestrogens, adaptogens, pumpkin seed, hops, sage, and amino acids—to promote hormonal harmony, bone integrity, mood stability, and cardiovascular comfort.
Why Synthetic Estrogens Are Used
Synthetic estrogens are primarily used for:
-
Combined hormonal birth control (e.g., pill, patch, ring)
-
Hormone replacement therapy (HRT) for menopause and perimenopause
In contraceptives, progestin prevents pregnancy, while estrogen stabilises bleeding, making menstrual cycles more predictable.
Common Types of Synthetic Estrogen
1. Ethinylestradiol
-
Most widely used in U.S. hormonal birth control
-
High bioavailability, meaning lower doses are effective
2. Estradiol Valerate
-
Converts into natural estradiol in the body
-
Found in newer contraceptive formulations
-
Helps reduce heavy menstrual bleeding
3. 17β-Estradiol (Bioidentical Estrogen)
-
Structurally identical to natural estrogen
-
Not commonly used in U.S. contraceptives due to low oral bioavailability
4. Conjugated Equine Estrogens
-
Derived from horse urine
-
Used in certain HRT products
Side Effects of Synthetic Estrogens
The effects vary based on individual biology, dosage, and the specific progestin paired with the estrogen.
Potential Side Effects (Combined Contraceptives)
-
Breast tenderness or cysts
-
Bloating or fluid retention
-
Nausea
-
Acne improvement
-
Irregular bleeding patterns
-
Altered cholesterol levels
-
Increased risk of blood clots and cardiovascular events
-
Slight increase in risk for breast and cervical cancers
-
Slight decrease in risk for endometrial and ovarian cancers
Potential Side Effects (Menopausal HRT)
-
Increased bone density
-
Higher risk of blood clots, stroke, and heart attack (especially with oral forms)
-
Small increased risk of gallbladder disease
-
Estrogen-alone therapy can increase the risk of endometrial cancer unless paired with progestin or used by those who have had a hysterectomy
Why Estrogen Form Matters
Choosing the right type of estrogen affects your health outcomes:
-
Ethinylestradiol is potent and commonly used
-
Estradiol Valerate may reduce bleeding and be gentler on the system
-
Natural estradiol (17β-estradiol) may lower clot risk but lacks widespread approval in contraceptives
Estrogen in Menopause and Perimenopause Treatment
Estrogen therapy helps alleviate symptoms like:
-
Hot flashes
-
Vaginal dryness
-
Night sweats
Forms Available:
-
Pills
-
Patches
-
Gels
-
Sprays
-
Creams
Adding progestins is crucial for individuals with a uterus to reduce the risk of endometrial hyperplasia or cancer.
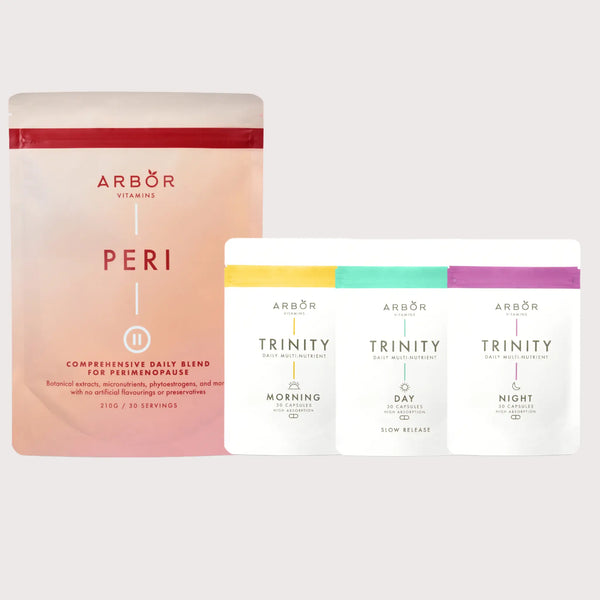
Non-hormonal support during perimenopause
Some individuals prefer or need alternatives to estrogen therapy. PERI Blend is a gentle, non-hormonal powder formulated for perimenopause—combining phytoestrogens (red clover, soy), adaptogens, amino acids (L‑Arginine, L‑Glutamine, L‑Lysine), herbs, and probiotics—to ease hot flashes, mood swings, energy dips, and menstrual irregularities
How to Know What You're Taking
Your medication packaging will list the active ingredients. In the U.S., combined hormonal contraceptives may include:
-
Ethinylestradiol
-
Estradiol valerate (less common)
If you're unsure, ask your healthcare provider or pharmacist.
Considering supplements?
If you’re using estrogen-based therapies (birth control or HRT), consider pairing them with targeted supplements. For instance, the PERI Blend supports perimenopausal balance, while the MENO Blend is designed to support women post-menopause with nutrients that complement hormone therapy. 
Final Thoughts: Making the Right Choice
Choosing to use hormonal contraception or hormone therapy is personal and should be tailored to your individual needs, health risks, and life goals.
If your current method isn’t working for you, don’t hesitate to explore other options. There is no one-size-fits-all approach when it comes to hormones.
Talk to your healthcare provider to assess your needs and determine what estrogen-based treatment (if any) is best for you.
Stay Informed, Stay Empowered
Knowledge is power. Understanding the different forms and effects of synthetic estrogens can help you make informed choices for your reproductive and hormonal health.
Explore non-hormonal support options
Empower your journey with tailored nutritional support. Visit ArborVitamins.com to learn more about PERI Blend for perimenopause and MENO Blend for postmenopause, both carefully formulated to work alongside your hormone strategy.

Disclaimer: This guide is for informational purposes only and does not constitute medical advice. Please consult a licensed healthcare professional before making any changes to your treatment plan.