As the age-old saying goes, "you are what you eat." Modern neuroscience, backed by rigorous research, is beginning to unravel how diet influences our mental health, confirming the profound connection between our food choices and brain function. Lets look into the neuroscientific connection between diet and mental health, shedding light on how specific nutrients and dietary patterns can shape mental health outcomes.
The Gut-Brain Axis: An Overview
At the epicenter of the diet-brain conversation is the gut-brain axis, a bidirectional communication channel between the gastrointestinal tract and the central nervous system. Recent advances in neurogastroenterology have shown that the gut microbiota plays a pivotal role in sending messages to the brain via the vagus nerve, influencing emotions, cognition, and even mental health conditions like depression.
Omega-3 Fatty Acids and Brain Health
Among the myriad of dietary components, omega-3 fatty acids, especially eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), hold a special place in neuroscientific research. Predominantly found in fatty fish, these compounds are integral to brain structure and function. Studies suggest that omega-3 supplementation might have neuroprotective properties, possibly attenuating symptoms of depression and anxiety.
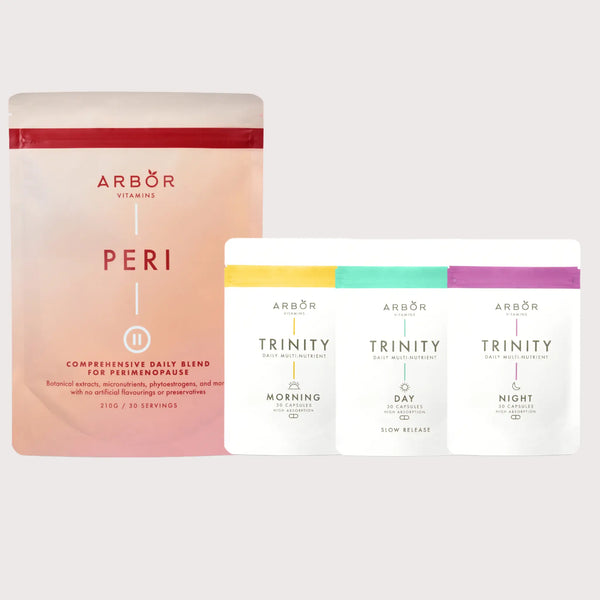
Shop now to heal yourself: Trinity Supplements
Micro- and Macronutrients: Beyond Omega-3s
-
Vitamin D: Once relegated to bone health, vitamin D is now understood as a key player in neurotransmitter synthesis. Emerging research links vitamin D deficiency with mood disorders.
-
B Vitamins: Integral for brain metabolism, B vitamins, particularly B12 and folate, are pivotal in neurotransmitter synthesis. Deficiencies can lead to mood disturbances and cognitive decline.
-
Tryptophan: An essential amino acid, tryptophan is a precursor to serotonin, the "feel-good" neurotransmitter. Its dietary intake might influence mood and emotional well-being.
Dietary Patterns and Mental Health
Beyond isolated nutrients, comprehensive dietary patterns play a significant role in mental health. The Mediterranean diet, characterised by whole grains, lean proteins, and an abundance of fruits and vegetables, has been associated with reduced depression risk. The mechanisms? Potentially through inflammation reduction, improved gut microbiota, and enhanced neuroplasticity.
Neuroinflammation: The Dietary LinkChronic inflammation is increasingly implicated in mental health disorders. Diets high in refined sugars and trans fats can exacerbate neuroinflammation, potentially leading to depressive symptoms. Anti-inflammatory diets, abundant in antioxidants and omega-3s, might offer protective benefits.
Conclusion
While the relationship between diet and mental health is complex and multifaceted, there's undeniable evidence of their interplay. As neuroscience continues to advance, it's becoming clear that dietary choices can profoundly influence brain health, offering a potential adjunctive approach to traditional mental health treatments.