Do Supplements Interact With Medications?
Written by a Clinical Pharmacist
Do supplements interact with medications? Yes. Certain vitamins, minerals, and herbal supplements can affect how prescription drugs are absorbed, metabolised, or function in the body.
Some supplements may:
-
Reduce medication absorption
-
Alter blood clotting
-
Influence blood sugar
-
Modify liver enzyme activity
That does not mean supplements are unsafe. It means the type, dose, and timing matter.
If you take medication — particularly blood thinners, diabetes treatments, thyroid medication, antibiotics, or immunosuppressants — understanding potential interactions is important.
Key Takeaway
Yes, supplements can interact with medications.
The most common mechanisms involve absorption competition, clotting effects, blood sugar overlap, and liver enzyme metabolism.
Most interactions are predictable and manageable with correct timing and medical guidance.
What Is a Supplement–Medication Interaction?
A supplement–medication interaction occurs when a vitamin, mineral, or herbal product alters how a prescription drug is absorbed, metabolised, or performs in the body.
Interactions may:
-
Reduce drug effectiveness
-
Increase side effects
-
Require dose adjustment
Most are dose-dependent and preventable.
Why Supplement–Medication Interactions Matter
Supplements are often perceived as “natural” and therefore harmless. Biologically, however, they are active compounds.
Vitamins and minerals can:
-
Compete for absorption pathways
-
Influence enzymes involved in drug metabolism
-
Affect clotting and blood sugar regulation
-
Alter gastric pH and gastrointestinal transit time
In many cases, interactions are manageable with appropriate spacing or formulation. In some cases, closer monitoring is required.
The key is not avoidance — it is informed use.
Quick Summary
The most common supplement–medication concerns involve:
-
Blood thinners (e.g. warfarin)
-
Diabetes medications
-
Thyroid medication
-
Certain antibiotics
-
Immunosuppressants
Below, we explain exactly how these interactions occur — and how to supplement safely.
🧬 Why Do Supplements Interact With Medications?
Supplements interact with medications for four main reasons:
-
They compete for absorption in the gut
-
They influence blood clotting pathways
-
They affect blood sugar regulation
-
They modify liver enzymes involved in drug metabolism
1️⃣ Absorption Competition (Most Common)
Some minerals bind to medications in the gut, reducing how much of the drug enters the bloodstream.
For example:
-
Iron can reduce absorption of levothyroxine and certain antibiotics
-
Magnesium and calcium can bind to tetracycline and fluoroquinolone antibiotics
-
Zinc may compete with other minerals when taken simultaneously
This usually requires separation rather than avoidance.
Spacing supplements 2–4 hours away from medication is often sufficient.
2️⃣ Blood Clotting Effects
Some nutrients influence clotting pathways.
-
Vitamin K directly affects clotting factors and can reduce the effectiveness of warfarin
-
High-dose vitamin E may increase bleeding tendency
-
Certain herbal extracts (e.g. ginkgo, garlic, high-dose omega-3s) may prolong bleeding time
For individuals on anticoagulants, consistency of intake is often more important than elimination.
3️⃣ Blood Sugar Regulation
Some supplements can lower blood glucose levels.
Examples include:
-
Magnesium
-
Chromium
-
Alpha-lipoic acid
-
Certain botanical extracts
When combined with diabetes medication, this may increase the risk of hypoglycaemia unless monitored.
4️⃣ Liver Enzyme Metabolism (CYP450 Pathways)
Many medications are processed through the cytochrome P450 enzyme system (CYP450) in the liver.
Substances that induce or inhibit these enzymes can alter circulating drug levels.
For example:
-
St John’s Wort can accelerate drug metabolism
-
Other herbal extracts may inhibit enzyme activity
This type of interaction can be clinically significant.
Herbal products should be treated with the same caution as pharmaceuticals.
Understanding the Different Types of Interactions
There is an important distinction between:
-
A direct drug interaction (e.g. vitamin K and warfarin)
-
A timing interaction (e.g. iron reducing absorption when taken together)
-
A physiological overlap (e.g. both supplement and medication lowering blood sugar)
Most supplement interactions fall into the second category — manageable with proper spacing and thoughtful formulation.
⚠️ Common Supplement–Medication Interactions
Below are well-documented examples:
| Supplement | Potential Interaction | Use Caution If Taking… | Why It Matters |
|---|---|---|---|
| Vitamin K | Reduces anticoagulant effect | Warfarin | May lower INR via clotting factor changes |
| Iron | Reduces medication absorption | Levothyroxine, tetracyclines | Binds in the gut and reduces uptake |
| Magnesium | Reduces medication absorption | Fluoroquinolones, bisphosphonates | Forms complexes that block absorption |
| Calcium | Reduces absorption | Thyroid meds, some antibiotics | Competes for transport pathways |
| High-dose Vitamin E | May increase bleeding tendency | Anticoagulants | Affects platelet aggregation |
| St John’s Wort | Alters drug metabolism | Antidepressants, oral contraceptives | Induces CYP enzymes, lowering drug levels |
| Chromium | May enhance glucose lowering | Insulin, metformin | Increases hypoglycaemia risk |
🛡 How to Supplement Safely When You’re on Medication
The goal is not to avoid supplements — it is to use them strategically.
1️⃣ Separate Timing
Spacing minerals 2–4 hours from medication often prevents absorption interference.
Particularly relevant for:
-
Thyroid medication
-
Antibiotics
-
Bisphosphonates
-
Osteoporosis treatments
2️⃣ Avoid Unnecessary Megadosing
Many documented interactions occur at higher-than-physiological doses.
A balanced approach is generally safer than high-dose single nutrients.
3️⃣ Maintain Consistency (Especially With Vitamin K)
If taking warfarin, avoid sudden changes in vitamin K intake. Stability supports consistent INR levels.
4️⃣ Consider Formulation Design
Large, single-tablet multivitamins often combine competing minerals (e.g. iron with calcium, zinc with copper).
While not a drug interaction, this may reduce internal absorption efficiency.
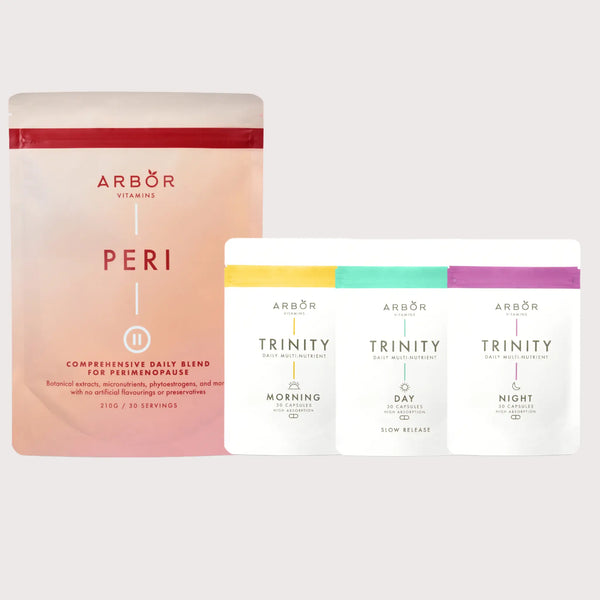
Structured AM/PM multinutrient systems such as Trinity (Arbor Vitamins’ three-part multivitamin system) are designed to separate competing minerals across the day rather than combining them into a single high-dose tablet.
Supplementation should always be individualised.

💡 When to Speak With Your Healthcare Provider
Consult your GP or pharmacist before introducing supplements if you:
-
Take anticoagulants
-
Use insulin or blood sugar-lowering medication
-
Are on thyroid replacement therapy
-
Take immunosuppressants
-
Are undergoing chemotherapy
-
Have kidney disease
Most interactions are manageable — but personal medical context matters.
🧠 Are Supplements Safe to Take With Medication?
In most cases, yes — when used appropriately.
Risk depends on:
-
The specific medication
-
The supplement dose
-
Timing of intake
-
Individual health status
With spacing, monitoring, and professional guidance, many supplements can be used safely alongside prescription medication.
🧠 Bottom Line
Yes, supplements can interact with medications.
But most interactions are:
-
Predictable
-
Dose-dependent
-
Manageable with spacing and consistency
The aim isn’t fear — it’s understanding.
When used thoughtfully, many vitamins and minerals can be incorporated safely alongside prescription medication.
This article is for educational purposes and does not replace personalised medical advice.
Last reviewed for clinical accuracy: February 2026.